Advancements in CAH Treatment: The Role of Crinecerfont in Reducing Corticosteroid Dependence
Share
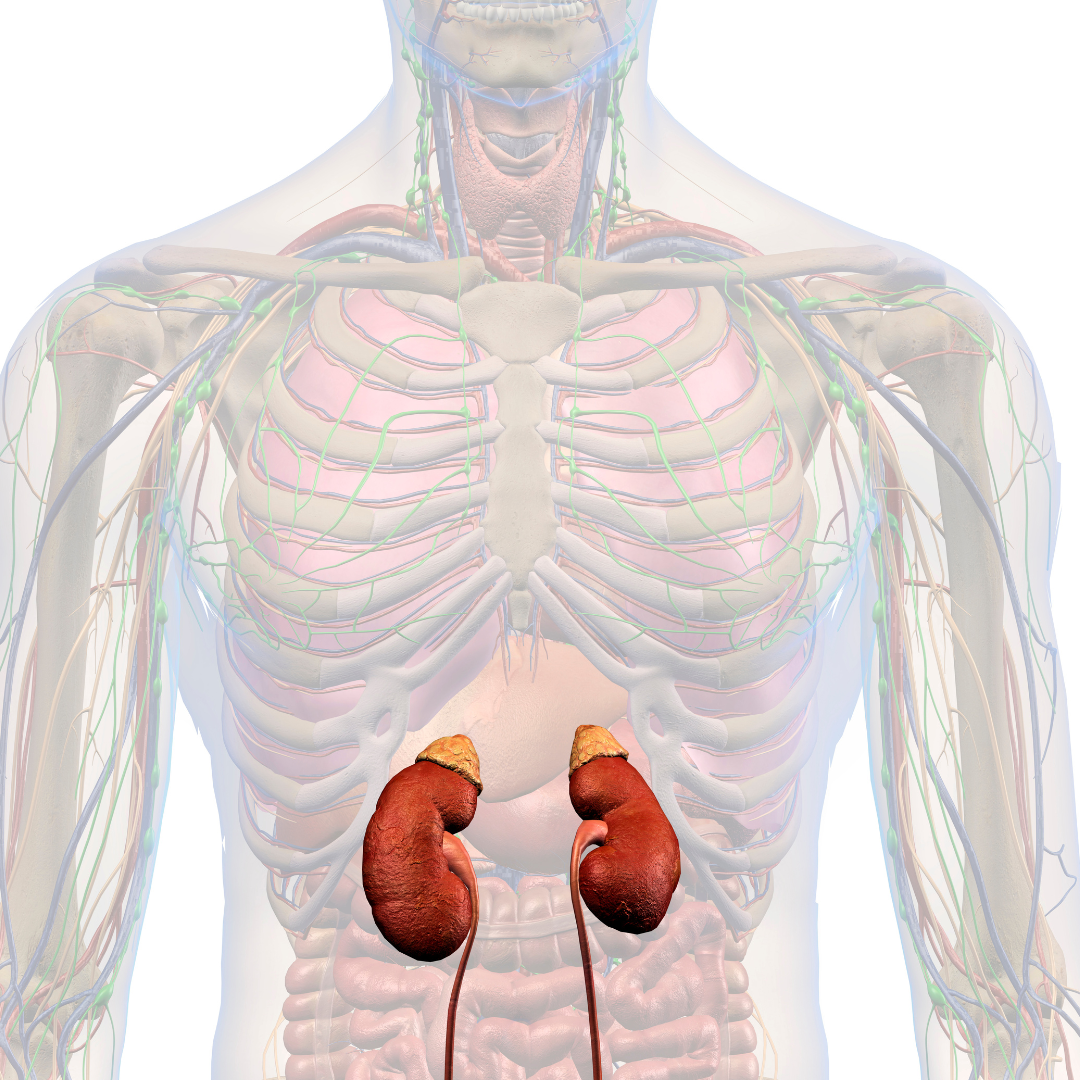
People born with the common form of congenital adrenal hyperplasia (CAH) lack an enzyme in the adrenal glands necessary for producing the hormones cortisol and aldosterone, which are crucial for stress response and blood pressure regulation.
In children with this rare condition, the adrenals redirect hormone production to create excess androgens, leading to early maturation, short stature, and infertility in adulthood.
Complicating matters, a simple stomach virus can trigger an adrenal crisis in CAH patients, causing shock if not treated immediately.
The standard treatment for children and adults with CAH involves high-dose corticosteroids, which come with significant side effects, including weight gain, diabetes, osteoporosis, and cognitive dysfunction.
A study led by Richard Auchus, M.D., Ph.D., from the U-M Medical School Department of Pharmacology and Internal Medicine, along with investigators from the CAHtalyst Adult Trial, provides strong evidence for an effective compound, crinecerfont, that could enable people with CAH to reduce their dose of replacement corticosteroids.
Published in the New England Journal of Medicine, the study randomized adults with CAH to take crinecerfont or a placebo along with their regular corticosteroid regimen.
A parallel study was conducted in children with CAH, and a companion paper reported those results.
After a month, patients on crinecerfont, but not on the placebo, experienced a reduction in the adrenal androgen, androstenedione, by half.
In the second part of the study, each group had their glucocorticoid dose gradually reduced.
The group on crinecerfont maintained a reduction in the adrenal hormone after 24 weeks with a glucocorticoid dose close to that naturally produced by the body.
“These patients are still cortisol deficient and will still need cortisol replacement, but with crinecerfont, they need much less and could be less likely to experience the long-term negative effects of current glucocorticoid dosing,” said Auchus.
In children with this rare condition, the adrenals redirect hormone production to create excess androgens, leading to early maturation, short stature, and infertility in adulthood.
Complicating matters, a simple stomach virus can trigger an adrenal crisis in CAH patients, causing shock if not treated immediately.
The standard treatment for children and adults with CAH involves high-dose corticosteroids, which come with significant side effects, including weight gain, diabetes, osteoporosis, and cognitive dysfunction.
A study led by Richard Auchus, M.D., Ph.D., from the U-M Medical School Department of Pharmacology and Internal Medicine, along with investigators from the CAHtalyst Adult Trial, provides strong evidence for an effective compound, crinecerfont, that could enable people with CAH to reduce their dose of replacement corticosteroids.
Published in the New England Journal of Medicine, the study randomized adults with CAH to take crinecerfont or a placebo along with their regular corticosteroid regimen.
A parallel study was conducted in children with CAH, and a companion paper reported those results.
After a month, patients on crinecerfont, but not on the placebo, experienced a reduction in the adrenal androgen, androstenedione, by half.
In the second part of the study, each group had their glucocorticoid dose gradually reduced.
The group on crinecerfont maintained a reduction in the adrenal hormone after 24 weeks with a glucocorticoid dose close to that naturally produced by the body.
“These patients are still cortisol deficient and will still need cortisol replacement, but with crinecerfont, they need much less and could be less likely to experience the long-term negative effects of current glucocorticoid dosing,” said Auchus.





